Unlike the other piped medical gases which are typically delivered to hospitals in cylinders, medical air is most often manufactured on-site. This is accomplished by pulling outside air into a medical air compressor which is connected to the piping system feeding the facility. Rarely, due to poor quality ambient air, medical air can be produced from blending compressed cylinder nitrogen and oxygen. Due to the large volume of air that most hospitals consume, on-site production is usually the most practical and economical method of supply. There is a down side, however, in that the equipment required to produce medical air suitable for patient use is quite complex and as such must be carefully installed and maintained to ensure that the risk of contamination or breakdown is kept to a minimum.
Most anesthesiologists are unaware of the complexity of the systems used to produce the medical air that they use. As medical air is considered by United States Pharmacopoeia to be a manufactured drug, anesthesiologists should be aware of the quality of the medical air produced in their facility and delivered to their patients. This article is meant to provide a basic understanding of a typical medical air system, including the purpose and operation of the key components. A familiarity with these basics should be sufficient to allow anesthesiologists to make inquires concerning the quality of the medical air delivered to their patients.
Medical air is used for a variety of patient applications. Many patients sensitive to oxygen toxicity are delivered air to lower their exposure to oxygen. Many of these patients have extremely delicate respiratory systems or processes which rely on a pure, accurate concentration of medical air. Some examples of patients dependent on a reliable, quality air supply would be neonates and those patients suffering from adult respiratory depression syndrome. Medical air is also used during anesthesia as a substitute for nitrous oxide to reduce the high concentration of oxygen exposure. While the source of medical air may be a manifold with a bank of compressed air cylinders, most hospitals use a compressor system. This article will refer to installations with air compressors. An illustration of a typical medical air plant is provided for your reference throughout this article’s discussion. To better understand the medical air system, we will follow the path of the air as it flows through the key components, from the source to the patient.
Start at the Source
The logical place to start learning about the medical air system is the intake pipe of the compressor. The intake is usually located on the facility’s roof. The intake location can have a major impact on the quality of the medical air produced. The location, design, and components of the air intake are described in National Fire Protection Association (NFPA) codes. NFPA 99, Standard for Health Care Facilities, recommendations for the design of medical gas systems are followed throughout the United States and will be referenced frequently in this article. However, you should be aware that local codes can supersede NFPA codes. NFPA 99 Sec. 4-3.1.9.2 states that the air intake shall be located outdoors above roof level, a minimum distance of 10 feet (3m) from any door, window, other intakes, or opening in the building, and a minimum distance of 20 feet above the ground. Intakes shall be turned down and screened or otherwise protected against entry of vermin or water with screening that shall be fabricated or composed of a non-corrosive material, such as stainless steel or other suitable materials. The NFPA allows flexibility when the roofs are staggered in height and suggests that factors such as the size of roofs, distance to nearest doors and windows, and the presence of other roof equipment can influence the final location. The intake need not always be higher than the highest roof.
In the case where there is more than one compressor system in the hospital, it is permissible to join pipes from separate compressors to one intake pipe which must be properly sized. However, the design must allow each compressor intake to be closed off by check valve, blind flange, or tube cap when a compressor is removed from service. This is meant to prevent mechanical room air from being drawn into the system from the open pipe.
The intake shall be labeled as the source of medical air. There has been a case where the medical air intake was located in the facilities heating ventilation air conditioning (HVAC) system. The coils on an HVAC system were being washed with an acidic solution for cleaning and maintenance. This resulted in fumes being unknowingly drawn into the medical air system and to the patients.
Air quality varies from region to region and even with proximity of your facility. For example, the air on the roof of a hospital located within a large city will not be as pure as air at a rural hospital. Yet, a rural facility’s air can be polluted by its proximity to a major highway, or the air intake placed too close to the medical vacuum system exhaust outlet. The latter is not an uncommon source of bacterial pollution where the gases from vacuum systems, literally of sewer quality, can be sucked into its medical air intake pipe. In older facilities the air intake may have been properly located and initially certified, but, there are cases where an intake became improperly located as the environment around the intake changed through facility expansion. Such has been the case with the addition of helicopter pads, parking lots, and truck loading docks where exhausts rich in carbon monoxide and engine pollutants were thus introduced in the manufacture of medical air.
The infamous “tweety bird” at the APSF scientific exhibit “Look Beyond the Walls” is an example of gross particulate contamination of a medical air supply. In this case, a bird was aspirated into the medical air compressor of a hospital and had occluded the system. The foul odor resulting from the decaying bird was a patient complaint that brought our committee member, Mr. Fred Evans, to service the system. Foul odor of any kind in a medical air system must be investigated. If the bird entered the system through an unscreened roof intake, the hospital was in violation of NFPA code. However, the entry was most likely through a break in the intake pipe which ran along a warehouse roof in course from the roof intake to the compressor. The break in pipeline continuity was a contractor error.
Interestingly, NFPA permits the intake to be within the building when the air source is equal or better than outside air, as filtered for use in operating rooms ventilating systems. It must be available twenty-four hours a day, seven days a week and periodically checked for purity. It is a good practice to test both the inside and outside air to occasionally determine if the inside air is of equal or better quality. Unless removed through the use of scrubbers or special filtration, any undesirable gases found in the atmosphere where the intake pipe is located will be compressed and delivered through the medical air system. Examples of this were covered at the beginning of the article.
Air Compressor and Its System
Inlet Filter/Muffler:
The air compressor process takes eight cubic feet of ambient air and compresses it into one cubic foot of compressed air. As a result, containments such as particulate matter, pollen, water, carbon monoxide, and breakdown materials of internal combustion engines or other containments are concentrated. Therefore, it is necessary to have methods in the manufacturing process to eliminate contaminates. The inlet filter/muffler should be located in the inlet side of the air compressor and can be part of some factory compressor packages. It is not uncommon for some systems to lack this filter since NFPA does not recognize it as a standard. Its primary function is to filter gross particulate from the ambient air aspirated through the screened intake usually located on the roof. It also acts as muffler for the air compressor to reduce noise pollution.
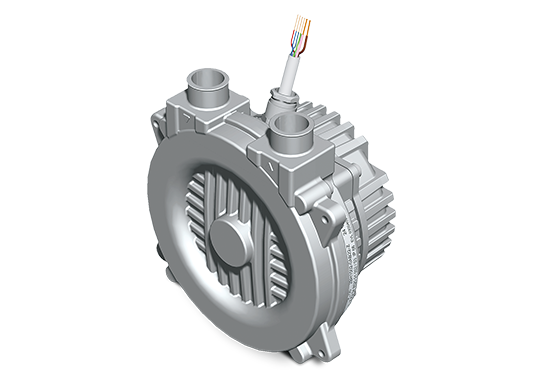
Air Compressor:
The air, usually from the atmosphere, is compressed by multiplexed medical air compressors, the “heart” of the medical air system. Two or more compressors (usually two) must be used for the support of medical air. Triplex and quadraplex systems are also available for facilities requiring greater demand. Simplex system components are not acceptable by NFPA 99. The duplication of much of the medical air systems provides a backup system if one unit breaks down or is in need of repair. The multiplexing provided by alternating units extends the life of the units and provides backup during demand overload. NFPA 99 requires that each unit separately must be capable of maintaining the supply of air at peak demand (NFPA 99 Sec. 4-3.9.1.2). Each compressor should be provided with an isolation valve, a pressure relief valve, and a check valve in its discharge line. Each compressor should be isolated from the system for servicing through an isolation (shut-off) valve in its discharge line. As stated in NFPA 99 Sec. 4-3.1.9.1, “The medical air compressors shall be designed to prevent the introduction of contaminants or liquid into the pipeline by: (a) Elimination of oil anywhere in the compressor, or (b) Separation of the oil-containing section by an open area to atmosphere, which allows continuous visual inspection of the interconnecting shaft.”There have been cases where non-medical grade compressors have been installed in hospitals which can create oils, water, and toxic oil breakdown products to mix with the medical air.
The medical air system is intended to produce gas used exclusively for breathable air delivered to patients through devices such as: flowmeters, blenders, anesthesia machines, and critical care ventilators. This would also include instruments that exhaust into the pharynx such as dental tools and pneumatically powered surgical tools. Medical air should not be used for non-medical applications such as powering pneumatic operated doors, engineering, or maintenance needs. As stated in NFPA 99, “As a compressed air supply source, a medical air compressor should not be used to supply air for other purposes because such use could increase service interruptions, reduced service life, and introduce additional opportunities for contamination.”
Aftercoolers (if required):
In larger air plants, aftercoolers may be desirable. Through the compression process air is heated and warmer air holds more moisture. Aftercoolers are used to reduce the temperature of the air after the compression process; this results in the precipitation of water. This water is then drained off. Aftercoolers should be duplexed so that one unit can handle 100% of the load. They should have water traps with automatic drains for water removal and isolation valves for servicing without the need to shut down the system. Although aftercoolers remove gross amounts of water they are not a substitute for dryers (see below).
Receiver:
The receiver is a large cylindrically shaped reservoir which stores a reserve volume of compressed air for usage. The receiver allows the efficient on/off operation of the compressors. Receivers are usually composed of iron and can be a source for rust particulate. Even though iron receivers meet NFPA standards, this material is subject to oxidation and flaking when introduced to moisture. Stainless steel receivers are available and should be installed during new construction, repair, or expansion despite the minimum NFPA standard. The receiver should be equipped with a pressure relief valve, site glass, pressure gauge, and a water trap with an automatic drain. The receiver should also be provided with a three valve bypass to allow servicing.
Air Dryers:
Dryers are an essential part of the system used to remove the water produced in the manufacturing process by the compression of ambient air which may be rich with humidity. Air dryers are usually of the refrigerant or desiccant type technology. Refrigerant dryers are an air-to-air refrigerant heat exchanger, a mechanical condensate separator, and an automatic drain trap. While desiccant dryers use an adsorption process to remove water, desiccant particulate can contaminate medical air if not properly maintained or filtered. The dryers should be duplexed so that only one dryer is used at one given time. Hence, each dryer should be capable of handling 100% of the load. They should also use bypass valves for isolation during servicing. Desiccant dryers are approximately 50% more expensive than refrigerant dryers.
Final Line Filters:
Important components of the medical air system are final line filters used to prevent introduction of particulate, oil, and odors from the medical air supply. Some contaminants may be introduced as hydrocarbons from leaking oil seals, spill-over from overloaded filters, rust flaking from a receiver, etc. NFPA 99 states, “Each of the filters shall be sized for 100% of the system peak calculated demand at design conditions and be rated for a minimum of 98% efficiency at 1 micron. These filters shall be equipped with a continuous visual indicator showing the status of the filter element life.” The need for visual indication was added by NFPA in 1993. The filters shall also be duplexed for isolation and shut down for servicing without completely shutting down the system. NFPA 99 recommends quarterly inspection of the filters. Some manufacturers provided filtration capabilities down to a .1 micron level. In environments with high concentrations of carbon monoxide special scrubbers may be introduced at this location to remove this or other pollutants.
Final Line Regulators:
Final line regulators should provide operating pressure for medical air throughout the facility at 50 to 55 psig. Whereas, the air compressor plant generates operating pressures of 80 to 100 psig. to facilitate the efficiency of the dryers. The regulators should be duplexed with isolation valves to allow servicing without the need to shut down the system. In Air Quality Monitoring as of the 1993 edition, NFPA 99 requires new construction to have continuous monitoring with central alarm capabilities for dew point and carbon monoxide contaminants downstream of the dryers and upstream of the piping system. These requirements have been largely driven by the water and elevated levels of carbon monoxide found in some medical gas systems.
Shut-off Valves:
The source shut-off valve should be located to permit the entire source of supply to be isolated from the piping system. This valve is located at the air compressor and its accessories downstream of the final line regulators. All shut-off valves should be quarter turn, specially cleaned, ball valves suitable for medical gas applications. The main supply shut-off valve should be located downstream of the source valve and outside of the enclosure, source room, or where the main line source first enters the building. The purpose of this valve is to shut off the supply in case of emergency or if the source valve is inaccessible. Each riser distributing gases to the above floors should have a shut-off valve adjacent to the riser connection. Each lateral branch or zone shall be provided with a shut-off valve which controls the flow of gases to the patient rooms on that branch. The branch/zone valve should allow the control of gases to that specific area and not effect the gas flow anywhere else in the system. Pressure gauges should be provided downstream of each lateral branch shut-off valve. NFPA 99 also states: “Anesthetizing locations and other vital life-support and critical areas, such as postanesthesia recovery, intensive care units, and coronary care units, shall be supplied directly from the riser without intervening valves…””A shut-off valve shall be located outside each anesthetizing location in each medical gas line, so located as to readily be accessible at all times for use in an emergency.” It is important that all shut-off valves be labeled with a caution, the name of the gas, and the location(s) which the valve controls. There have been numerous incidents of medical gases being shut off due to poor labeling (if any) of the valve and the locations which it supplies.
Alarms:
An automatic pressure switch shall be located downstream of the main supply line shut-off valve. A visual and audible alarm should indicate a rise or fall of the main line pressure above or below the nominal line pressure. The alarm should be located where it is continuously monitored throughout the facility’s time of operation. NFPA 99 states, “Area alarms shall be provided for anesthetizing locations and critical care areas. Warning signals shall be provided for all medical gas piping systems supplying these areas…” The area alarm in the anesthetizing location is intended to monitor all locations on a single branch, not each individual operating room.
Piping:
Piping which is used for the system downstream of the source shut-off valve shall be composed of copper. NFPA states: “Piping shall be hard-drawn seamless medical gas tube Type K or L (ASTM B819), and bear one of the following markings: OXY, MED, OXY/MED, ACR/OXY, or ACR/MED.” Medical air pipes are to be of the same material and quality as oxygen pipes.
The type of material used with the compressors and with the piping system shall be non-corrosive. Copper and brass are most commonly used. The pipe bringing air from the outside intake to the compressor should be non-corrosive since it is exposed to moisture and atmospheric contaminants. Although the NFPA does not spell out the intake pipe’s specific composition, as it does for the compressor and the pipeline downstream, the intake pipe should not be iron. It is not uncommon to find the plumbing contractors engaged to install medical piping to treat the piping as ordinary water or sewer plumbing. Galvanized steel is also unacceptable since the zinc plating could flake off under the pressure and flow of gases.
A recent (1995) major hospital inspection was found to have iron piping between the medical air compressor, dryers, receiver, and aftercoolers. The system had been certified as meeting NFPA codes seven years earlier. The correction of such design errors can be expensive. It is far more reasonable for the anesthesiologists to be aware of basic construction codes and have a say in proper installation from the beginning. Iron and galvanized pipe may oxidize, resulting in particulate matter flaking off from the pressure and flow, and will result in being carried downstream where it may interfere with the flow of gases or proper operation of station outlets, ventilators, blenders, anesthesia systems, or other pieces of secondary equipment.
Station Patient/Outlets:
Station outlets consist of primary and secondary check valves which allow secondary pieces of equipment to be attached to the medical gas line. Station outlets should be used only for the delivery of gases intended for medical use. The outlet shall also be designed as being gas specific by using size or keyed dissimilar connections specific for each individual gas. Each outlet shall be labeled with the name or chemical symbol and the specific color coding for the gas supplied.
More on Contaminants and Particulates:
Water is the most common contaminant found in medical air lines and is perhaps the most insidious of the contaminants found. It can also cause some of the most costly damage to secondary equipment. Water, unlike particulate, can pass through particulate filters and make its way into anesthesia machines, ventilators, other commonly used secondary equipment, and the patient as well. Jerry Lavene, Manager of the Anesthesia Vaporizer Repair Center from Ohmeda, states “The most common contaminant we find in vaporizers during their disassemble for remanufacture is moisture. Moisture or the combined effects of moisture with the anesthetic agent can create issues within the internal mechanisms of the vaporizer.” Some critical care ventilators saturated with water were non-repairable and had to be scraped by one facility. The anesthesia machines required a complete overhaul to restore them to usable condition. The presence of water can also provide the medium for bacterial growth. Water located in medical air lines which are subjected to low temperatures can freeze and occlude gas flow. Water can also facilitate the oxidation of the copper piping inside the medical air line.
Water may be introduced through a variety of ways. Inadequate removal of water through undersized, saturated, or the lack of appropriate air dryers is common. Water may be introduced through malfunctioning liquid ring air compressor components. Failure of automatic drains in aftercoolers, receivers, dryers, or other components of the medical air plant is an area of frequent fault allowing unwanted water into the system.
Oils can be introduced through a non-medical grade air compressor being installed. This may occur through improper equipment specification or purchasing. Medical grade compressors have been known to fail and introduce oil into the system. Some medical air compressors are now available which use a totally oil-less compressor technology to prevent this possibility. Don’t assume the air compressor being used for your facility is suitable for medical grade air. The possibility of oil contamination has resulted in hydrocarbon monitoring requirements.
Construction debris such as sand, solder, flux, dirt, vermin, and so on have been found in medical air lines due to poor techniques in the construction process. These particulates can be introduced downstream of the filtration system located at the medical air plant. This can be avoided through proper design, installation procedures and techniques, and final testing (certification) of the new system or addition. There are processes available to remove these contaminants found in existing systems. Medical air is an important life sustaining gas commonly used in our facilities. Anesthesiologists should be aware of those responsible for overseeing the medical air system and their qualifications. During construction they should be aware of design and installation specifications. Preventative maintenance programs should be in place and the results of as many as 17 tests performed at required intervals should be reviewed and evaluated.
Vigilance will result in patients receiving clean and safe medical air. Ask yourself, “Would you want your family placed on your present medical air system?”